7 min read
Intelligence Will Change Everything in Healthcare…If It Has the Data
 Stan Schneider
:
May 15, 2024
Stan Schneider
:
May 15, 2024
The Future of Healthcare is Intelligent
Healthcare professionals and device manufacturers love to complain about how slow the industry changes. I disagree. Change may be incremental and almost imperceptible, but the accumulated effect is nothing short of transformative. You just have to step back and look at what’s really different. Over time, healthcare makes slow—but stunning—progress.
Over the last few decades many new technologies became common in hospitals: Imaging… Patient monitoring... Electronic health records (EHRs)... Robotic surgery... Telemedicine... These changed everything. The hospital experience today is nothing like it was only 30 years ago. Today, it’s entirely possible to enter a hospital, see a new doctor who is fully aware of your medical history, get a high resolution CT scan, undergo a robotically-assisted surgery, enter a monitored recovery ward, and go home with remotely-connected instruments and telemedicine support. None of these things…none of these things…was practical only 30 years ago. That’s the result of the “slow” industry change, accumulating into the most profound period of advances in healthcare science and practice in history.
Why? The answer is both simple and profound: all these transformations stem from advancements in computing. The exponential increase in compute power, pervasive networking, and data integration are making systems smarter. And smart systems drive better patient outcomes.
And now, the news is full of hype about AI’s potential to impact every industry. Healthcare, one of the most expensive and least-automated industries, stands out as a tempting target. The way we analyze, monitor, treat, and care for patients is mostly manual, error-prone, and inefficient. To put it bluntly, intelligence is sorely needed in healthcare. But it can’t happen yet. Data is the key to intelligence, and the data isn’t there.
Data availability is a key blocker to smarter healthcare. Clinical data flow is demanding; enterprise IT and cloud systems can’t provide the information fast enough or reliably enough to operate physical systems. Intelligent clinical systems need more than stale “collected” data. They need to get coordinated information from multiple instruments to AI algorithms and back to the care team or treatment systems fast enough to support life-critical care. Implementing intelligent healthcare without relevant data to understand the patient is like driving a car without a windshield to see the road. Intelligent healthcare requires seamless interoperability of data flow across integrated devices and systems. Getting the right data to the right place at the right time is critical.
The Potential
Just imagine the potential…
- What if imaging systems could automatically diagnose orthopedic issues, design 3-D printable replacement joints, and then install those designs with a robotic surgical system?
- What if patient monitoring could replace sporadic human check-ins with real-time detection and prediction of problems by correlating multiple instruments?
- What if EHRs were constantly updated with every event, waveform, or reading from patient monitoring, diagnostics, and treatments…and then could combine patient history with current conditions to make better decisions in real time?
- What if patients in remote locations could benefit from expertise anywhere in the world by enabling remote human assistance and robotic operation?
The real potential is for AI technology to become a key enabler, or even the key enabler, of better clinical efficiency, of better use of scarce medical personnel, and of better care. AI can lower costs by relieving harried care teams of repetitive drudgery, eliminate many errors by automating error checking, and drive healthcare equity by augmenting local talent with learned expertise. AI can be the single biggest improvement to healthcare in history. Technology can truly join the care team.
Let's look at two promising advances: Intelligent patient monitoring and robotic surgery.
Intelligent patient monitoring
Although monitoring is arguably the greatest technological advent in 30 years, it can’t today help with diagnosis without someone watching it. No single instrument provides enough information to understand the patient’s condition, but there’s no easy way to correlate the readings. The various instruments don’t even know they are connected to the same patient. Because a single instrument may have many reasons for unexpected data, false alarms are rampant (and usually turned off). Today’s patient monitoring systems are a collection of independent readings with no potential for smarter analysis.
There is an EHR record, but it’s not useful for care. Connections to the database are far too slow, incomplete, and unsynchronized to be useful for diagnosis. For instance, the medical records likely have only vitals (e.g., heart rate), not the waveforms needed for diagnosis. Instrument clocks aren’t even synchronized, eliminating the ability to even do post-analysis. To check a patient, you have to physically walk into the room or the telemetry nurses’ station and look at the outputs from each machine live. To record the waveform, all you can do is print it on paper, scan it, and put that image in the EHR. There’s simply not enough data flow to make the system smart.
So, doctors and nurses run from room to room looking at displays every hour or so to make decisions. It’s inefficient, and it’s not good enough to optimize patient outcomes. As a result, surgical patients are 1,000 times more likely to die in post-op than on the operating table. It’s not that they suddenly decline or the monitoring instruments fail. It’s because the sporadic deep analysis of the data by harried care teams isn’t fast enough to catch even a slow decline over time.
Imagine if instead monitors were wireless, instruments could work together, and data was available for intelligent automated analysis. You could connect your patient to monitors and track them around the hospital. You could take a look at patient status on your iPad and prescribe medication from anywhere: the ward, your office, or the cafeteria. Even better, the high-quality data from many instruments would enable AIs to watch for signs of trouble every millisecond. Rather than just enable the care team, technology would join the care team.
It goes beyond single patients, of course. The hospital could also use this to measure and optimize care. For instance, if the hospital wants to better understand sepsis mortality, the system could make a projection score, deciding if a patient may be septic before the doctors can figure it out. Then, it can use the data and outcomes to improve care.
I didn’t choose this scenario randomly. This magic, wireless, intelligent system already exists, the result of a decade of development by GE Healthcare. The Portrait Mobile system is wireless, with no connectors. It supports multiple coordinated instruments associated with the patient. It delivers the right data to advanced algorithms to provide intelligent alarming and detect patient problems. It’s truly a transformation in healthcare technology.
But it wasn’t easy. Portrait Mobile has to work 24x7 over any hospital network. It has to scale, preserve data, register patients, and protect privacy. It has to run on battery, seamlessly traverse networks, tolerate faults, and combine many different types of devices that come and go at any time. It has to be fast, secure, and reliable. It has to provide patient history review. It has to be easy to use in a dynamic clinical environment. It must filter and deliver voracious data demands to the analytics algorithms. It has to run for days, months, and years without error. And it has to do all this while always getting the right data to the right place at the right time.
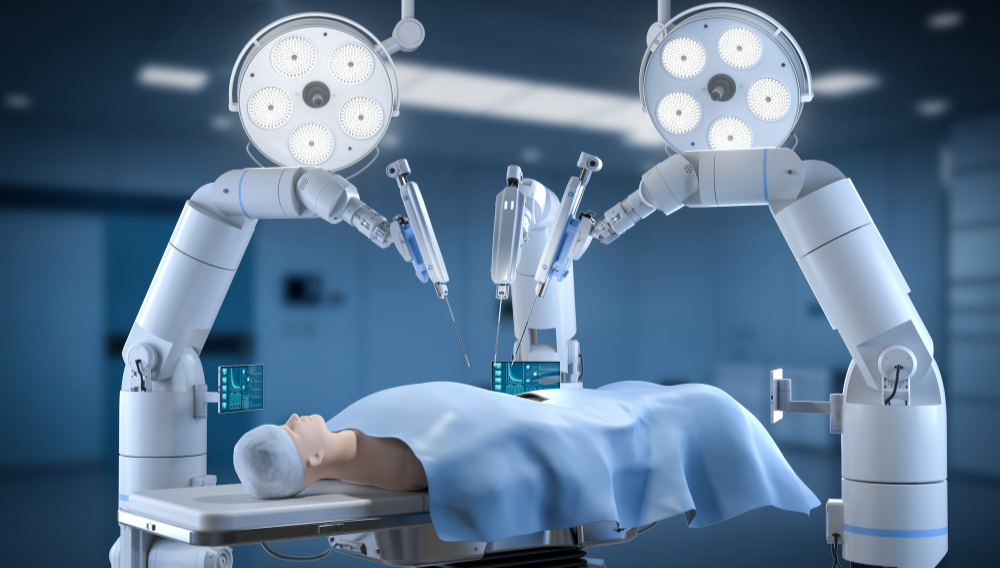
Surgical Robotics
As another example, consider knee replacement surgery. Compared to only a few years ago, prosthetic knees are commonplace these days. In fact, it’s become so common that efficiency is critical; surgeons handle almost 1 million operations in the U.S. each year. Today, these are manual operations. But specialized robotic systems will soon change both the process and economics of these procedures.
Successful knee replacement requires accuracy. The biomechanics have to be right, balancing many factors to enable the proper gait. In this process, making accurate cuts is by far the hardest and most important step. It can take 2-3 hours just to correctly position all the things required for the surgery. Setup, cut planning, and evaluation drive much of the cost and risk. Still, in the end, humans aren’t good at precision. Even trained surgeons can’t make perfect angled cuts. And adapting the variety of human bones to standard parts means most patients don’t get an optimal result.
Robotics can help this. Robots can follow extremely precise cut paths generated by the imaging and CAD plans. The resulting precision angles and ultra-smooth surfaces are so clean that many operations don’t require cement; the part is press fit and the bone grows into the part like a natural joint. With robotic accuracy and flexibility, custom joints become realistic to install. Instead of adapting the patient to a standard part, a custom part can be 3D printed from the imaging information. Manually adapting procedures to install these unique parts is impractical for humans. It’s entirely possible for a robot.
Of course, it’s not quite that simple. Importantly, the robot has to know exactly where the bone is, a process called “registration.” That’s done with an imaging system that can track something that looks like an antenna with reflective targets on it. This is attached (screwed into) the bone, and then another probe with targets on it is used to locate bone points exactly. After that, the vision system knows exactly where the bone is while it’s cutting.
Then, to make it all work, the right data has to get to the right place at the right time. The vision system communicates where the bone is, even if it’s moving. The surgeon controls when and how fast to cut. The robot uses those to execute a perfect cut along the pre-planned angle. This is all so automated that it can even be done remotely, even with the surgeon thousands of miles away. It’s a bold new intelligent world.
The knee-replacement robot essentially copies how surgeons work, but with better precision and efficiency. Increasing evidence shows that the results of robotic joint replacement are better. The robotic surgery in these studies improved implant positioning, alignment, and ligament balance.
A glimpse of the future
These are just two of thousands of potential applications of intelligent medical care. They both integrate advanced computing and intelligence to change the very nature of procedures and care. They share information from many sources, combining AI or smart algorithms with advanced sensing, detailed 3D models from scanners, precision motors, electronic health records, and more. And they are pioneering applications.
Developing intelligent medical systems costs millions of dollars and takes many years. Stakes for patients and care teams are high. Every advance must be tested, tuned, approved, and maintained. Developing AI-driven medical systems is expensive, slow, and risky. But progress is undeniable.
Healthcare, as always, makes slow—but stunning—progress. Prepare to be stunned.
—
This blog is courtesy of RTI, the largest provider of infrastructure software for smart-world systems. We provide the distributed data flow capabilities that connect sensors, motors, people, and intelligent algorithms together. It’s an inspiring time to be a key driver of the smart world.
About the author:
 Stan Schneider is CEO of Real-Time Innovations (RTI), the largest software framework provider for smart machine and real-world systems.
Stan Schneider is CEO of Real-Time Innovations (RTI), the largest software framework provider for smart machine and real-world systems.
Stan also serves on the advisory board for IoT Solutions World Congress and the boards of the Teleoperations Consortium and the Autonomous Vehicle Computing Consortium (AVCC). Stan holds a PhD in EE/CS from Stanford University.
Posts by Tag
- Developers/Engineer (177)
- Connext DDS Suite (77)
- Technology (74)
- News & Events (73)
- 2020 (54)
- Standards & Consortia (51)
- Aerospace & Defense (48)
- Automotive (35)
- 2023 (34)
- 2022 (29)
- IIoT (27)
- Leadership (24)
- 2024 (22)
- Cybersecurity (20)
- Healthcare (20)
- 2021 (19)
- Connectivity Technology (15)
- Military Avionics (15)
- Culture & Careers (14)
- FACE (13)
- Connext DDS Pro (10)
- JADC2 (10)
- ROS 2 (10)
- 2025 (7)
- Connext DDS Tools (7)
- Connext DDS Micro (6)
- Databus (6)
- Transportation (5)
- Case + Code (4)
- Connext DDS (4)
- Connext DDS Cert (4)
- Energy Systems (4)
- FACE Technical Standard (4)
- Oil & Gas (3)
- RTI Labs (3)
- Research (3)
- Robotics (3)
- #A&D (2)
- Connext Conference (2)
- Edge Computing (2)
- MDO (2)
- MS&T (2)
- TSN (2)
- ABMS (1)
- C4ISR (1)
- ISO 26262 (1)
- L3Harris (1)
- LabView (1)
- MathWorks (1)
- National Instruments (1)
- Simulation (1)
- Tech Talks (1)
- UAM (1)
- Videos (1)
- eVTOL (1)
 Success-Plan Services
Success-Plan Services